
Weight loss surgery physically alters the stomach size, reducing the amount of food it can hold. A popular option for weight loss surgery is the gastric sleeve, which reduces the stomach size by about 80%, fundamentally changing how much you can eat and how you need to approach every aspect of nutrition and meal planning for the rest of your life.
Creating an effective menu gastric sleeve meal plan requires understanding that this surgery transforms your entire relationship with food. What I’ve learned the hard way is that the mental stuff is honestly just as tough as the physical changes. Success isn’t just about following rules – it’s about figuring out strategies that work with your new reality, even when that reality feels weird and frustrating sometimes.
Table of Contents
- Rewiring Your Brain’s Food Relationship After Surgery
- Making Every Bite Count When Your Stomach’s Tiny
- Stealing Smart Strategies from the Gastric Bypass Community
- Timing Your Meals Like a Metabolic Pro
- Breaking Through Plateaus and Long-Term Success
TL;DR
- Your brain needs just as much retraining as your stomach, and it’s honestly harder than anyone tells you
- Every single bite must pack maximum nutritional punch when you can only eat 2-4 ounces (yes, it’s as limiting as it sounds)
- Gastric bypass patients have figured out some brilliant tricks that work for us too
- When you eat matters almost as much as what you eat, though it takes time to figure out your rhythm
- Plateaus are normal and they suck, but you can work through them with strategic planning
- Social eating becomes awkward as hell and requires honest communication (and sometimes white lies)
- Supplement timing matters more than you’d think, and yes, you’ll probably mess it up at first
Rewiring Your Brain’s Food Relationship After Surgery
Getting a gastric sleeve isn’t just about shrinking your stomach – it completely changes how your brain processes hunger, fullness, and food cravings. Look, I’m not gonna sugarcoat this: the mental game is way harder than the physical restrictions. Your brain spent decades learning how to eat, and it doesn’t just forget overnight because you had surgery.
You’ll need specific strategies to retrain your brain’s relationship with food while navigating social situations that revolve around eating. The way your brain rewires itself after gastric sleeve surgery affects way more than just appetite signals. Your brain’s reward pathways, emotional eating triggers, and even food memories need deliberate work to change.
Understanding these changes helps you work with your new anatomy instead of fighting against old patterns that no longer serve you (though you’ll probably fight them anyway for a while – we all do). When developing your new eating patterns, understanding how intermittent fasting principles work can help you establish healthy meal timing even with your reduced capacity.
Your Brain on Sleeve: Understanding the Mental Shift
The transformation goes deeper than physical hunger signals. I discovered that my brain’s reward system had to completely recalibrate after surgery. Foods that once triggered happy feelings suddenly felt overwhelming or just… meh. This isn’t a bug in the system – it’s actually something you can learn to work with, though it feels super weird at first.
Your emotional eating patterns don’t automatically disappear when your stomach shrinks. I found myself reaching for food during stress even when I physically couldn’t eat more than a few bites. The disconnect between wanting to stress-eat a whole pizza and only being able to handle three crackers creates this unique kind of frustration that nobody really prepares you for.
The 20-Minute Mindful Eating Reset
This approach retrains your brain to recognize the new, much subtler fullness signals your sleeve sends. Most of us eat way too fast and miss these crucial cues, leading to that awful “stuck” feeling or throwing up (yeah, it happens to most of us at least a few times).
Here’s what actually works (though it feels ridiculous at first):
- Set your phone timer for 20-30 minutes per meal (I know, I know, it seems excessive)
- Put your fork down between every single bite (this will drive you crazy initially)
- Chew each bite 25-30 times before swallowing (count if you have to)
- Take three deep breaths after bites 4, 8, and 12
Sarah, three months post-surgery, was constantly getting that uncomfortable “stuck” feeling after meals. She started using the 20-minute timer method and realized she was inhaling her entire portion in under 5 minutes. By forcing herself to slow down and actually put her fork down between bites, she eliminated the discomfort and found she felt satisfied with half the food she was previously trying to force down.
The gastric bypass community has used similar timing techniques for years, and they work for us too. The key difference is that we can usually tolerate slightly faster eating once we’ve mastered the basics (though “fast” is still pretty slow compared to normal people).
Mapping Your Emotional Food Triggers
Creating a personal inventory of which foods trigger emotional eating helps you develop alternative coping mechanisms before you’re in crisis mode. This isn’t about willpower – that’s basically useless when you’re stressed and want comfort food.
The process that actually helped me (even though I resisted it at first):
- Keep a detailed 14-day food and emotion journal (yes, write it down, your memory lies to you)
- Look for patterns between your emotional state and food choices
- Create a specific “replacement ritual” for each trigger food
- Practice your replacement ritual for 21 days straight to build new pathways in your brain
I realized that my 3 PM energy crash always made me crave crunchy, salty foods. Instead of fighting the craving (which never worked anyway), I developed a replacement ritual: five minutes of deep breathing followed by a small portion of roasted chickpeas. The crunch satisfied whatever my brain was looking for while giving me protein and fiber my sleeve could actually handle.
Handling Social Eating Without Losing Your Mind
Social situations become incredibly awkward when you can only eat a few bites while everyone else is having full meals. I’m not gonna lie – I’ve definitely excused myself to cry in restaurant bathrooms because I felt so different and broken. Having prepared explanations and alternative suggestions makes these situations way less stressful for everyone involved.
According to Banner Health, registered dietitian Lauren Pellizzon emphasizes that “The biggest misconception about eating after bariatric surgery is that people need to be on a ‘diet.’ The truth is that you need to adopt permanent lifestyle changes to be successful long-term. Diets are short-term and generally difficult to stick with. Lifestyle changes are permanent and more easily managed.”
This perspective shift helped me reframe social eating challenges. I wasn’t on some restrictive diet – I was living with new anatomy that required different approaches. That mindset helped, though some days it still sucks watching everyone else finish their meals.
The Three-Level Explanation System
Having different explanations ready for different relationships prevents you from over-sharing with acquaintances or under-explaining to close family who need to understand your needs (and who will probably still try to push food on you anyway).
What I wish someone had told me:
- Prepare three different explanation levels (casual acquaintance, close friend, family)
- Practice explaining your needs in 30 seconds or less
- Suggest alternative social activities that don’t center on large meals
- Master ordering appetizers as main courses without feeling weird about it
For casual acquaintances, I simply say “I have a small appetite and prefer to eat slowly.” Close friends get more detail about my surgery and specific needs. Family members receive full education about my new anatomy and how they can support my success (though honestly, some of them still don’t get it).
Decoding Your New Hunger Signals
Learning to distinguish between true physiological hunger, head hunger, and your sleeve’s new fullness signals takes practice and a lot of trial and error. The old “empty stomach growling” hunger rarely happens anymore, so you need new ways to figure out when and how much to eat.
Your sleeve creates entirely different hunger and satiety signals than your original stomach. I had to learn that the absence of hunger doesn’t mean I shouldn’t eat, and the presence of mild fullness means I should definitely stop (even if my brain is screaming that three bites isn’t a real meal).
The Traffic Light Hunger Check
This real-time assessment system helps you make informed eating decisions throughout the day instead of eating out of habit or boredom (which we all still do sometimes).
The system that keeps me on track (most days):
- Check in with your body every 2 hours using this system
- Green: True hunger with energy dip – time to eat
- Yellow: Mild interest in food, possibly thirst or habit – wait 30 minutes
- Red: No hunger, eating would be purely emotional – find another activity
The traffic light system prevents both under-eating (which slows metabolism) and over-eating (which makes you feel awful). I set phone reminders for the first month until the check-ins became automatic. Some days I still ignore the signals, but at least now I know I’m doing it.
Making Every Bite Count When Your Stomach’s Tiny
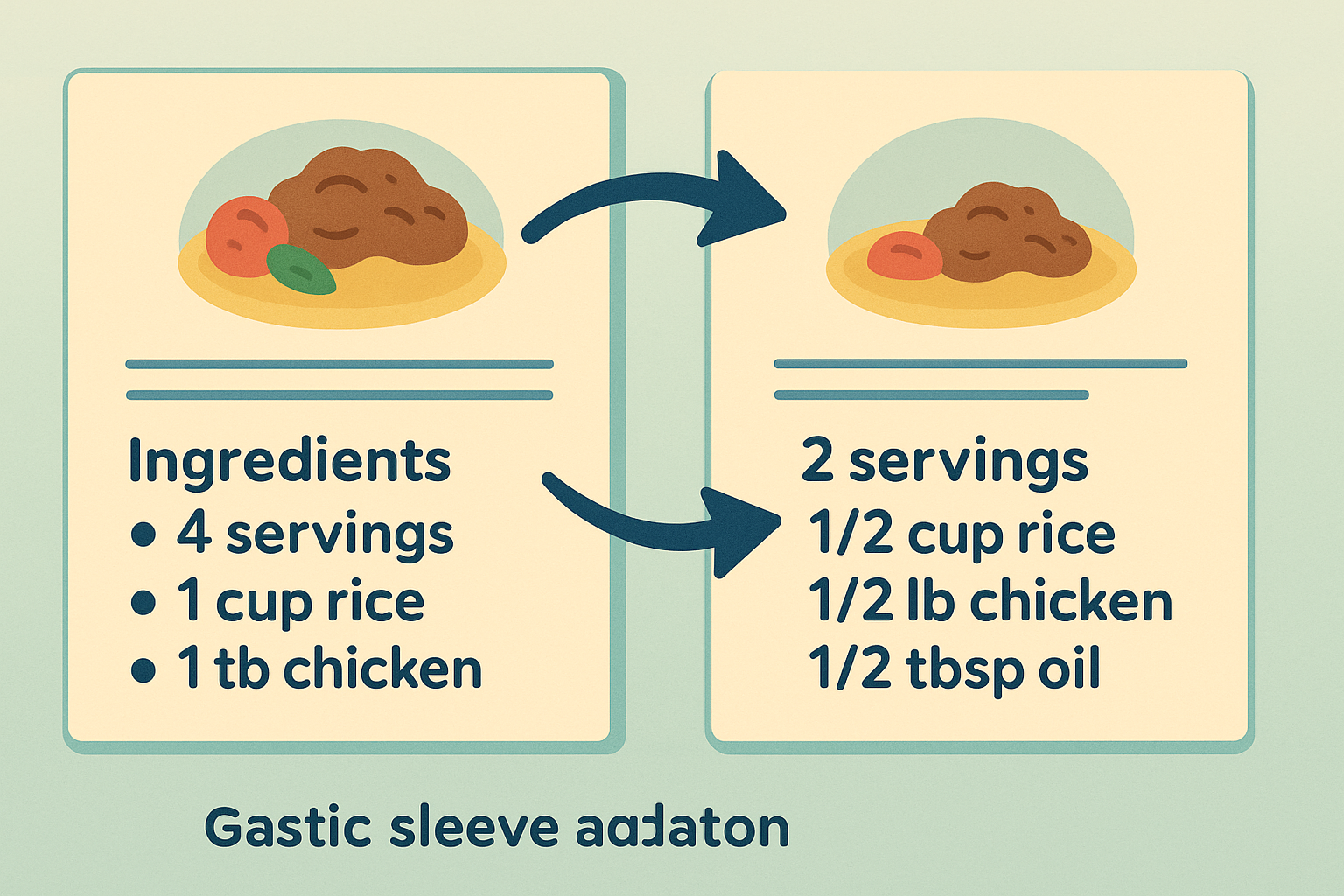
With your stomach capacity reduced to about 2-4 ounces, every single bite needs to deliver maximum nutritional value. This means completely reimagining how you think about meal composition, food preparation, and nutrient absorption. I had to learn that eating smarter matters way more than ever before, which honestly feels overwhelming sometimes.
After surgery, eating smaller portions is easy because it takes less food to feel full. Understanding portion sizes helps you achieve your weight loss goals and maintain them in the future. Most patients can consistently eat 1/2 cup or four to six ounces of food at six months after surgery, making every bite crucial for meeting nutritional needs.
The challenge isn’t just eating less – it’s making sure that your dramatically reduced food intake still provides all the nutrients your body needs to function. I discovered that this requires a completely different approach to meal planning and food selection, plus a lot of supplements that I’m still figuring out.

Since your body’s ability to absorb nutrients becomes crucial, implementing strategies to improve digestion becomes essential for maximizing the nutritional value of every meal.
Maximizing Nutrient Absorption from Tiny Portions
Your body’s ability to absorb nutrients from smaller food quantities can be optimized through strategic food combinations and preparation methods. These techniques help ensure you’re getting the most nutritional bang for your buck from every meal, though honestly, some of them feel like a lot of work.
I learned that absorption isn’t just about what you eat – it’s about how you prepare your digestive system to receive and process nutrients. The gastric bypass community has mastered these techniques out of necessity, and we can adapt their strategies for our better absorption capacity.
Priming Your Digestive System Before Meals
These pre-meal practices activate your digestive system for maximum nutrient extraction from the limited food volume you can consume. Fair warning: some of these taste pretty awful at first.
What works (and what doesn’t):
- Drink 1 tablespoon apple cider vinegar in 4 oz water 15 minutes before meals (it tastes terrible but works)
- Include 2-3 tablespoons of fermented foods at the start of each meal
- Chew fresh ginger or take ginger supplements 10 minutes before eating
- Practice 2 minutes of deep breathing before meals to activate your nervous system’s “rest and digest” mode
Apple cider vinegar can be particularly beneficial for gastric sleeve patients, as drinking vinegars support gut health and may enhance nutrient absorption from your limited food intake.
The deep breathing component surprised me with how well it worked. When your nervous system is in “rest and digest” mode, your stomach produces more digestive enzymes and your intestines absorb nutrients more efficiently. Plus, it gives you a moment to actually think about what you’re about to eat.
Building Your Plate for Maximum Absorption
This systematic approach to meal construction maximizes nutrient absorption while respecting your sleeve’s capacity limitations. The order matters more than you’d think, though it feels pretty rigid at first.
The layering strategy that changed my results:
- Start with 2-3 oz of lean protein as your foundation
- Add 1-2 tablespoons of healthy fats to enhance fat-soluble vitamin absorption
- Include 2-3 tablespoons of colorful vegetables for micronutrients
- Add complex carbohydrates only if you have space remaining
This prioritization ensures that even if you can’t finish your entire portion (which happens more often than you’d think), you’ve consumed the most critical nutrients first. I used to fill up on vegetables and then have no room for protein – completely backwards for optimal nutrition and honestly pretty frustrating.
Creating Your Personal Nutrient Density Map
Developing personalized meal templates based on your individual nutrient needs and absorption capabilities helps ensure you’re meeting your nutritional requirements despite eating much smaller quantities. This sounds super nerdy, but it’s actually pretty helpful once you get the hang of it.
Your nutrient needs don’t decrease proportionally with your food intake. You still need the same vitamins, minerals, and essential fatty acids, but now you have to get them from a fraction of the food volume. It’s like trying to fit a full-sized wardrobe into a tiny closet.
The Nutrient-Per-Bite Calculator
Look, I know this sounds super nerdy, but I literally started writing the protein amounts on sticky notes and putting them on my fridge. This method helps you evaluate and optimize the nutritional value of every food choice within your limited capacity. Whatever works, right?
How to build your system:
- Calculate protein, vitamin, and mineral content per ounce of your regular foods
- Create a “top 20” list of your most nutrient-dense options
- Rotate through this list to ensure variety while maximizing nutrition
- Track your energy levels and adjust based on how different foods make you feel
Mike discovered that 1 oz of salmon provided 7g protein, omega-3s, and B12, while 1 oz of chicken breast gave him 8g protein but fewer micronutrients. By creating his nutrient-per-bite calculator, he realized rotating between salmon, sardines, and grass-fed beef gave him more nutritional variety than sticking to just chicken, even though chicken had slightly higher protein per ounce.
Working with Seasonal Nutrition Cycles
Adapting your meal plan to leverage seasonal produce peaks ensures maximum micronutrient diversity throughout the year while keeping your meals interesting and varied. Plus, it gives you something to look forward to when eating the same tiny portions gets boring.
The seasonal strategy:
- Research your local growing seasons and peak nutrient times for different vegetables
- Plan quarterly menu rotations based on seasonal availability
- Learn proper freezing and fermentation techniques to preserve peak-season nutrients
- Supplement strategically during off-seasons for your most important nutrients
I started buying vegetables at their peak season and learning preservation techniques. Frozen blueberries in January still provide more antioxidants than fresh berries shipped from thousands of miles away. This approach keeps my limited vegetable portions as nutrient-dense as possible year-round, and honestly makes me feel like I’m doing something right.

Stealing Smart Strategies from the Gastric Bypass Community
The gastric bypass community has been dealing with absorption challenges and tiny portions longer than us sleeve patients, and they’ve developed some brilliant strategies we can adapt. Understanding how sleeve surgery differs from bypass helps you cherry-pick the best techniques while avoiding approaches that don’t work for your anatomy.
Bypass patients face malabsorption issues that we don’t have, but their solutions for maximizing nutrition from minimal food intake are pure gold. I’ve spent months lurking in their online communities and adapting their most effective strategies, though some of their restrictions seem way more intense than what we deal with.
The gastric bypass diet protocols have been refined through decades of trial and error. We can benefit from their hard-won wisdom while adjusting for our better absorption capacity.
Understanding the Absorption Advantage
Sleeve patients have better absorption than bypass patients, but we can still benefit from their hard-learned lessons about preventing nutrient deficiencies and maximizing supplement effectiveness. Basically, they’ve done the heavy lifting on figuring out what works.
Our intact intestinal tract means we absorb nutrients more efficiently than bypass patients, but we still face challenges from dramatically reduced food volume. This gives us opportunities to modify their strategies for even better results, though it still takes some experimenting.
Adapting Bypass Supplement Protocols
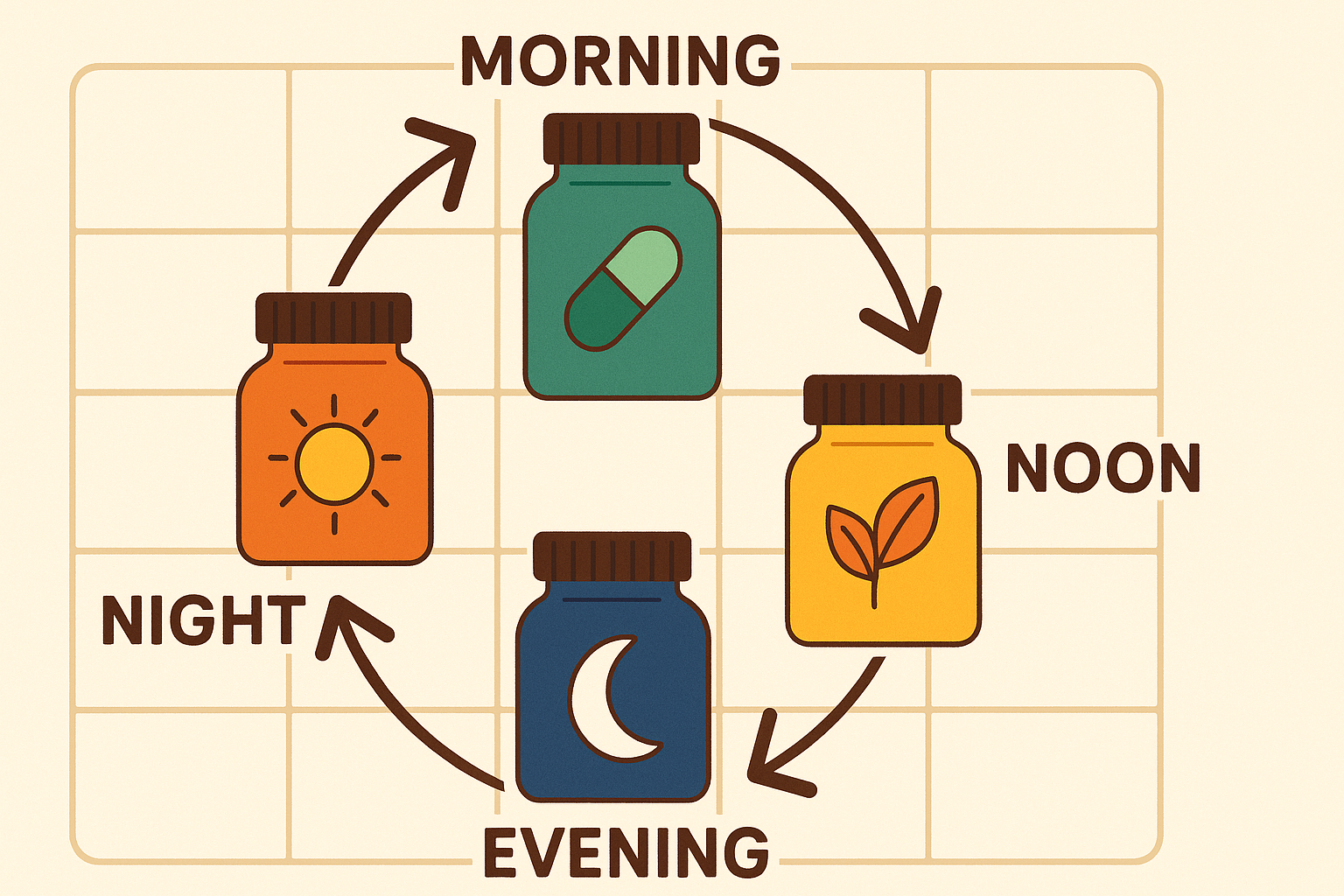
Using modified versions of gastric bypass supplement schedules helps prevent nutrient deficiencies before they become problems, even though sleeve patients don’t have the same malabsorption issues. It’s like insurance for your nutrition.
What I’ve adapted from the bypass community:
- Modified B12 supplementation schedule (monthly instead of weekly)
- Quarterly iron level monitoring with adjusted supplementation
- Proven food combination strategies for optimal absorption
- Vitamin D3 with K2 supplementation approach
According to Bedfordshire Hospitals NHS, patients should aim for at least 1.5 litres of fluid per day, and it’s emphasized that “staying well hydrated is important, aim for at least 1.5 litres of fluid per day. Try carrying a bottle of water with you and take frequent sips. Avoid drinking with food as the fluid can fill up your stomach.”
This hydration guidance applies to both bypass and sleeve patients, but I’ve found that sleeve patients can sometimes tolerate small sips with meals better than the strict separation bypass patients require. Though honestly, I still forget to drink enough water most days.
Learning from Cross-Surgery Communities
Tapping into the collective wisdom of various bariatric surgery communities provides access to tested strategies and recipes that can be modified for sleeve-specific needs. These people have figured out some really clever workarounds.
When adapting recipes from other bariatric communities, understanding which supplements are essential daily helps ensure you’re meeting nutritional needs regardless of your meal plan variations.
Recipe Modification for Sleeve Patients
This systematic approach to adapting gastric bypass recipes accounts for sleeve patients’ different tolerance levels and better absorption rates. It took me probably six different attempts to get this right.
The adaptation process:
- Start with proven gastric bypass recipes as your foundation
- Adjust portion sizes upward by 25-30% to account for better absorption
- Increase healthy fat content slightly since you can absorb fats normally
- Test modifications in small batches and document your body’s responses
I discovered that many gastric bypass diet recipes were too restrictive for my sleeve anatomy. Their cauliflower mash recipe called for zero butter, but I could handle a tablespoon of grass-fed butter for better fat-soluble vitamin absorption and improved taste (because let’s be honest, plain cauliflower mash is pretty sad).
The bypass community’s protein-forward casseroles work brilliantly for meal prep. I make their tuna and white bean salad but increase the olive oil from 1 teaspoon to 1 tablespoon per serving. My sleeve tolerates the extra fat well, and it helps me absorb more nutrients from the vegetables.
Timing Your Meals Like a Metabolic Pro
When you eat can be just as important as what you eat for maximizing weight loss, energy levels, and overall health outcomes. Strategic meal timing, intermittent fasting, and working with your body’s natural rhythms can significantly boost your results post-surgery. I’ve learned that working with your body’s natural patterns makes everything easier, though it takes time to figure out your personal rhythm.
Your sleeve surgery changes more than just stomach capacity – it affects hormone production, insulin sensitivity, and metabolic rate. Timing becomes crucial when you’re working with such limited food volume, plus you have to figure out what actually works for your schedule.
Syncing Your Eating with Your Body’s Natural Rhythms
Aligning your eating schedule with hormonal rhythms optimizes weight loss, energy levels, and overall health outcomes. Your body has natural peaks and valleys for processing different nutrients throughout the day, though honestly, this stuff can feel pretty overwhelming when you’re just trying to get enough protein.
Cortisol peaks in the morning, making it the ideal time for your largest meal. Insulin sensitivity is highest upon waking, which means your body can handle carbohydrates more effectively early in the day. Growth hormone releases during deep sleep, but only if you’re not digesting food.
The Metabolic Window Strategy
This time-based eating approach maximizes your body’s ability to process nutrients and maintain steady energy throughout the day by working with your natural insulin sensitivity patterns. It sounds fancy, but it’s basically just eating your biggest meal in the morning.
The timing that works (most of the time):
- Eat your largest meal within 2 hours of waking when insulin sensitivity peaks
- Space meals 3-4 hours apart to allow complete gastric emptying
- Stop eating 3-4 hours before bedtime to optimize sleep and growth hormone release
- Track your energy patterns for 2 weeks and adjust timing based on your individual preferences
| Time Period | Meal Type | Portion Size | Key Focus |
|---|---|---|---|
| Within 2 hours of waking | Largest meal | 1/2 – 3/4 cup | High protein, complex carbs |
| 3-4 hours later | Mid-meal | 1/4 – 1/2 cup | Protein + vegetables |
| 3-4 hours later | Final meal | 1/4 – 1/2 cup | Protein + healthy fats |
| Evening | Optional snack | 2-3 tbsp | Protein only if needed |
This schedule prevents the energy crashes that come from eating tiny amounts throughout the day. Your sleeve can handle larger portions in the morning when your metabolism is primed for fuel, though “larger” is still pretty small compared to normal people.
Smart Intermittent Fasting for Sleeve Patients
Safely incorporating intermittent fasting principles while ensuring adequate nutrition within your sleeve’s constraints requires careful planning and gradual implementation. Don’t try to go from eating every few hours to fasting for 16 hours overnight – that’s a recipe for disaster.
How to do it safely:
- Start with a 12-hour eating window and gradually reduce to 8-10 hours over 4 weeks
- Focus on nutrient timing rather than calorie restriction during eating windows
- Monitor protein intake carefully to ensure you meet daily requirements
- Break fasts with easily digestible proteins to optimize absorption
Many gastric bypass diet plans inadvertently create intermittent fasting patterns due to eating restrictions. We can be more intentional about it while ensuring adequate nutrition, though it takes some experimentation to find what works.
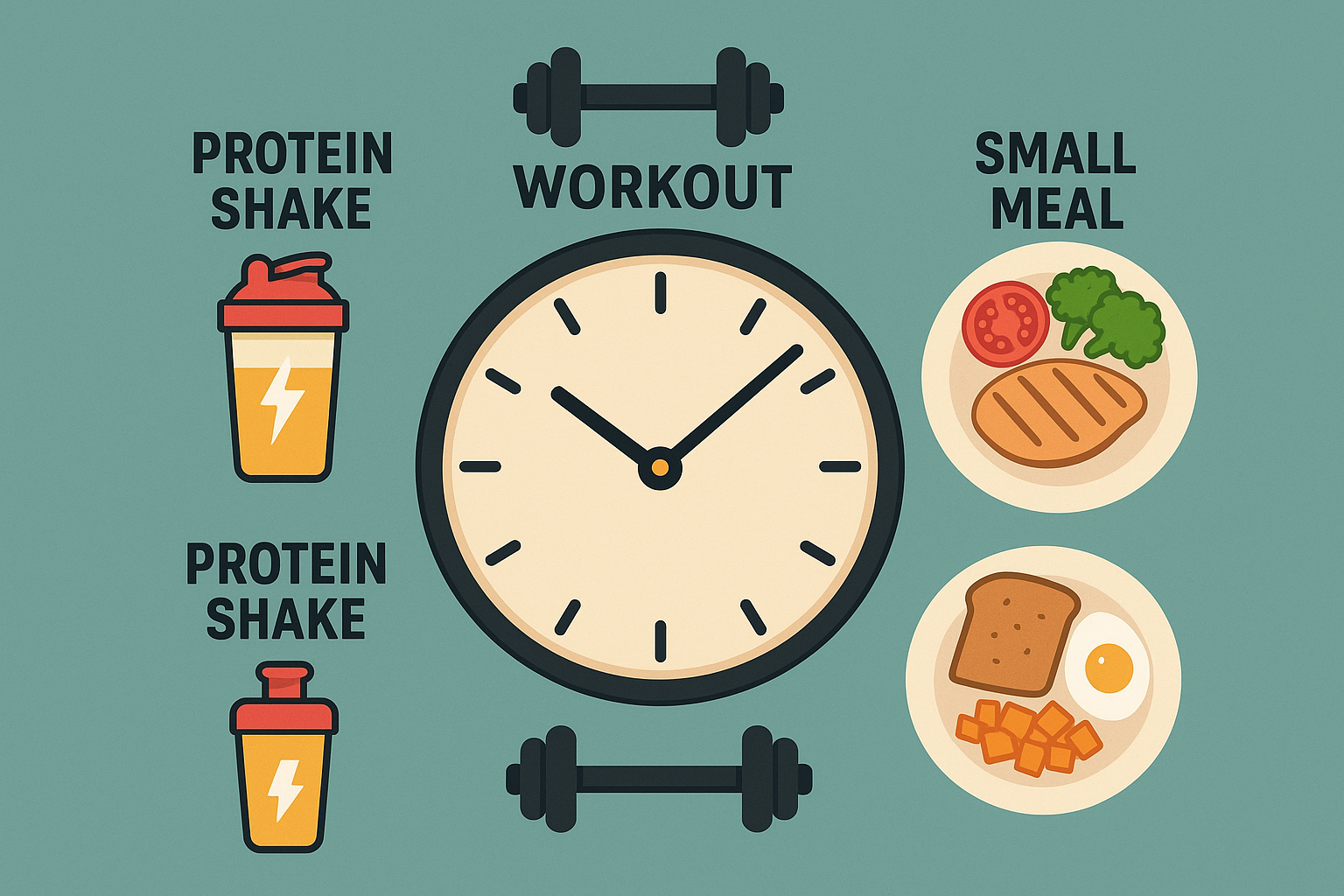
Coordinating Exercise and Nutrition
Timing your meals around workouts maximizes both exercise performance and recovery while working within your sleeve’s limitations. The key is finding what works with your reduced capacity, which honestly took me months to figure out.
Exercise timing becomes tricky when you can only eat small amounts. I had to experiment extensively to find the sweet spot between having enough energy for workouts and not feeling sick from eating too close to exercise (spoiler alert: I threw up after workouts more than once).
Pre and Post-Workout Nutrition That Actually Works
These specialized feeding strategies fuel your workouts and optimize recovery without overwhelming your reduced stomach capacity or causing discomfort during exercise. It’s a delicate balance that requires some trial and error.
What I’ve learned through lots of trial and error:
- Consume 15-20g of easily digestible protein 30-45 minutes before workouts
- Focus on liquid nutrition immediately post-workout for faster absorption
- Plan your largest meal within 2 hours post-workout for optimal recovery
- Experiment with different protein sources to find what your sleeve tolerates during active periods
Greek yogurt with a scoop of protein powder works perfectly pre-workout for me. It provides sustained energy without the heavy feeling that solid foods create. Post-workout, I drink a protein shake within 15 minutes, then eat my largest solid meal 90 minutes later when my appetite returns and I can actually handle solid food again.
Breaking Through Plateaus and Long-Term Success
Developing adaptive strategies to maintain weight loss momentum and metabolic health becomes crucial as your body adjusts to its new anatomy over months and years. Plateaus are normal and expected, but they suck and feel like you’re doing something wrong when you’re not. You can work through them with strategic interventions and long-term planning that evolves with your changing needs.
Your metabolism will adapt to your new eating patterns within 6-12 months post-surgery. This adaptation is your body’s survival mechanism, but it can stall weight loss progress and make you feel like you’re broken. The gastric bypass community has developed sophisticated approaches to prevent and break through these plateaus.
Training Your Metabolism to Stay Flexible
Teaching your transformed digestive system to efficiently process different macronutrient ratios prevents the metabolic slowdown that often occurs 12-18 months post-surgery. Basically, you’re trying to trick your metabolism into not getting too comfortable.
Your body becomes incredibly efficient at extracting energy from whatever fuel you consistently provide. This efficiency can work against continued weight loss if you don’t periodically challenge your metabolism with strategic variations, though honestly, some days you just want to eat the same thing without thinking about it.
Carb Cycling for Sleeve Patients
This structured approach to varying carbohydrate intake prevents metabolic adaptation while working within your sleeve’s capacity constraints. It keeps your metabolism guessing without overwhelming your system, though it requires more planning than I initially wanted to do.
The cycling approach:
- Establish baseline carb tolerance through 2 weeks of consistent 20-30g daily intake
- Implement weekly cycles: 3 days low-carb (15-20g), 2 days moderate (30-40g), 2 days higher (50-60g)
- Monitor weight, energy, and cravings throughout each cycle
- Adjust ratios based on your individual response patterns
Since one year post-op, the patient’s portion sizes increase to what they will remain for the long term – usually 1 to 1 1/2 cups or 8 to 12 oz of food, this becomes the perfect time to implement strategic carb cycling without overwhelming your system.
Understanding how to find your carb tolerance becomes especially important for sleeve patients who need to optimize their limited capacity for maximum results.
Strategic Protein Rotation
Systematically varying protein sources prevents food intolerances and maintains optimal amino acid profiles as your digestive system continues adapting over time. Plus, it keeps you from getting completely bored with chicken breast every single day.
The rotation system:
- Create a 4-week protein rotation schedule using 8-10 different sources
- Introduce one new protein source every 2 weeks to assess tolerance
- Track digestive comfort, satiety levels, and energy with each protein type
- Build your personalized “tolerance hierarchy” for long-term meal planning
I noticed that eating chicken breast daily for months led to decreased satisfaction and digestive issues. Rotating between fish, eggs, lean beef, and plant proteins every few days restored my appetite and improved my energy levels significantly. It also made meals way less boring.
Plateau-Breaking Protocols That Work
Evidence-based interventions can restart weight loss when your body reaches adaptive plateaus, which commonly occur 6-24 months post-surgery. These aren’t extreme measures – they’re strategic resets, though they can feel pretty intense when you’re used to your routine.
Plateaus feel frustrating as hell, but they’re actually signs that your body has successfully adapted to your new anatomy. The challenge is convincing your metabolism that it’s safe to continue releasing stored energy, which sometimes requires getting creative.
Metabolic Reset Techniques
These strategic dietary and lifestyle modifications restart sluggish metabolism without compromising nutritional status or triggering regain patterns. They’re basically ways to shake things up when your body gets too comfortable.
The reset strategies:
- Implement a 5-day “basically tricking your metabolism” protocol alternating high and low-calorie days
- Increase meal frequency to 5-6 mini-meals for 2 weeks to boost the energy boost from eating
- Add 10-15 minutes of high-intensity interval training 3x weekly
- Incorporate cold exposure therapy (cold showers, ice baths) to activate brown fat
Jennifer hit a 6-month plateau despite following her meal plan perfectly. She implemented the metabolic confusion protocol, alternating between 800-calorie days and 1200-calorie days for one week. After about two weeks of trying this (and wanting to quit multiple times), Jennifer finally saw the scale move again. She learned that her body had adapted to her consistent 1000-calorie intake, and the variation “woke up” her metabolism without requiring extreme restriction.
For those interested in cold exposure benefits, understanding cold shower health benefits can provide additional motivation to incorporate this plateau-breaking technique, though honestly, cold showers suck at first.
Smart Supplement Cycling
Strategic use of metabolism-supporting supplements in cycles prevents adaptation and maintains effectiveness over time. Your body gets used to everything eventually, supplements included.
The cycling approach:
- Rotate between different thermogenic supplements every 6-8 weeks
- Cycle digestive enzymes on/off monthly to prevent dependency
- Use adaptogens in 12-week cycles with 4-week breaks
- Time supplement cycles with seasonal changes and stress levels
Green tea extract worked brilliantly for my first plateau, but after 8 weeks, I noticed diminishing returns. Switching to cayenne pepper supplements for 6 weeks, then back to green tea, maintained the metabolic boost without adaptation. I’m still figuring out the timing thing, honestly.
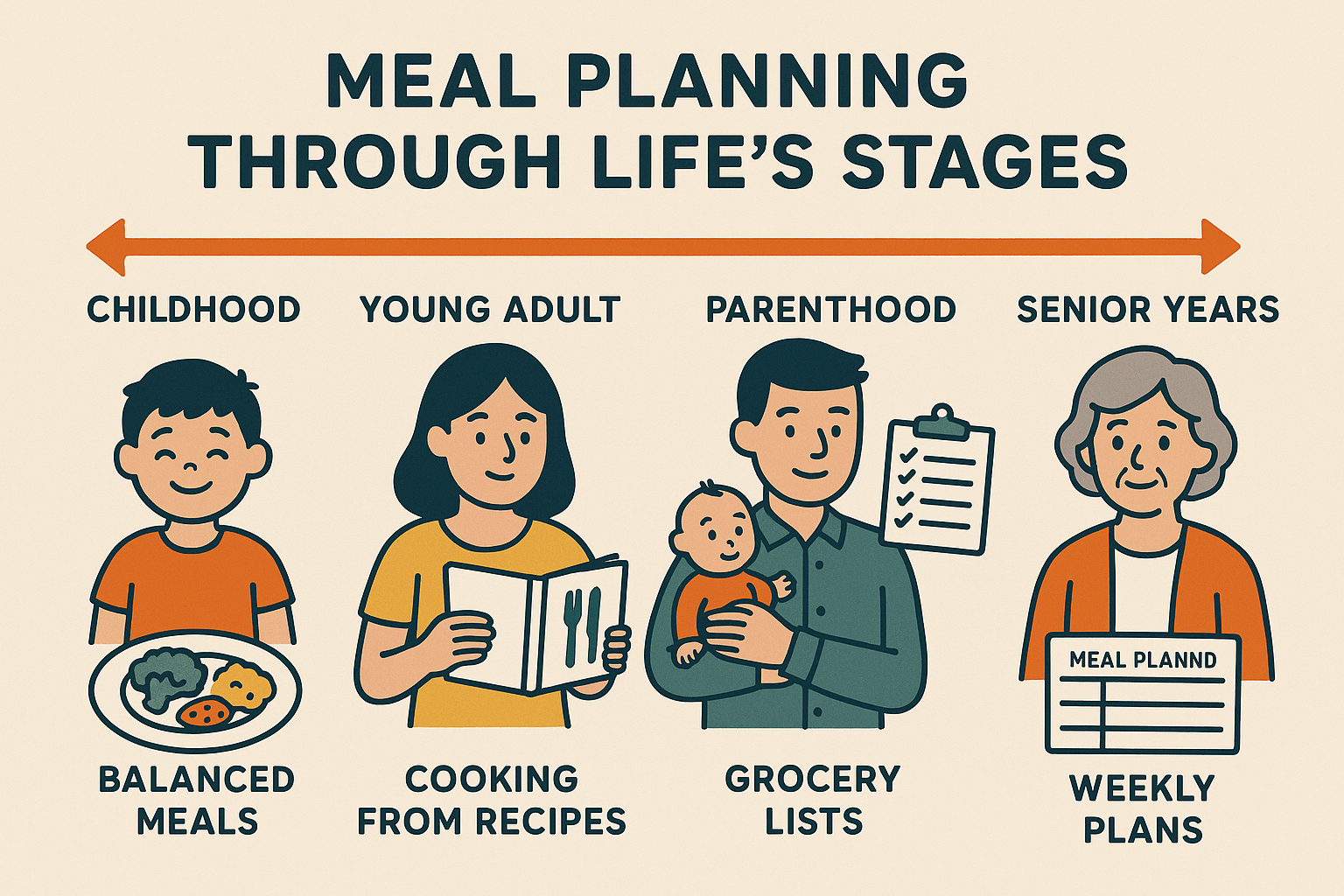
Advanced Planning for Life Changes
Developing increasingly sophisticated meal planning approaches becomes important as you master the basics and your needs evolve with lifestyle changes, aging, and metabolic shifts. Your nutritional needs will change, and your system needs to be flexible enough to adapt.
Your nutritional needs will change as you age, face stress, deal with illness, and navigate life transitions. Building flexibility into your meal planning system prevents these changes from derailing your progress, though you’ll probably still have some rough patches.
Precision Tracking Beyond Calories
Moving beyond basic calorie counting to track biomarkers, energy patterns, and body composition changes enables truly personalized nutrition optimization. This sounds super intense, but it’s actually pretty helpful once you get into it.
The advanced tracking approach:
- Invest in regular body composition analysis (DEXA or InBody scans quarterly)
- Track HbA1c, inflammatory markers, and micronutrient levels bi-annually
- Use continuous glucose monitoring for 2-week periods to understand food responses
- Correlate subjective energy ratings with objective biomarker changes
I discovered through continuous glucose monitoring that sweet potatoes spiked my blood sugar more than white potatoes, completely contrary to conventional wisdom. This data helped me make better carbohydrate choices within my limited capacity, though it was kind of annoying to discover I’d been avoiding the “wrong” potato.

Adapting for Life Transitions
Modifying your meal planning approach for major life transitions, hormonal changes, and aging while maintaining the benefits of your sleeve surgery requires ongoing adjustment. Life doesn’t stop just because you had surgery. Life stage modifications:
- Adjust protein requirements upward during perimenopause/andropause
- Modify meal timing and composition during high-stress periods
- Increase anti-inflammatory foods during illness or injury recovery
- Plan for travel, holidays, and social events with portable nutrition strategies
During a particularly stressful work period, I increased my magnesium intake and shifted to more frequent, smaller meals to support my adrenal function. These temporary adjustments prevented stress-related weight regain while supporting my overall health, though I definitely wasn’t perfect about it.
Speaking of nutrition support during your gastric sleeve journey, Organic Authority offers high-quality collagen supplements that can help bridge nutritional gaps when your food intake is limited. Their carefully sourced collagen provides easily absorbed protein that works well with sleeve restrictions – perfect for those times when you need extra protein support but can’t handle solid foods.
When considering collagen supplementation, understanding whether collagen supplements actually work helps you make informed decisions about adding them to your post-surgery nutrition plan.
Final Thoughts
Creating a successful menu gastric sleeve meal plan goes way beyond just eating smaller portions. I’ve learned that the mental game, nutrient optimization, strategic timing, and long-term adaptation strategies are just as important as the food choices themselves. Your relationship with food will never be the same after surgery, and honestly, that’s both liberating and terrifying at the same time.
The key is approaching this journey with patience, flexibility, and a willingness to experiment. What works for someone else might not work for you, and what works for you now might need adjustment in six months. That’s completely normal and expected, even though it can feel frustrating when you just want a simple answer.
Remember that plateaus aren’t failures – they’re opportunities to reassess and refine your approach, even though they suck and make you feel like you’re doing something wrong. Your body is incredibly adaptive, which means you need to stay one step ahead with strategic changes to your meal planning, timing, and supplement protocols.
Most importantly, don’t try to do everything at once. Pick one or two strategies from this guide and master them before adding more complexity. Your sleeve surgery was just the beginning – the real transformation happens through consistent, thoughtful choices over months and years.
Some days will still be hard, even years later. You’ll probably always have to think about food differently than other people. There are days when I still miss being able to stress-eat a whole pizza or share a big meal with friends without feeling weird about it. But honestly? Most days it feels normal now, and that’s pretty amazing. You don’t have to be perfect at this – none of us are.

