
Look, if you’ve dealt with gastritis, you already know that big meals feel like torture. There’s actually science behind why – research shows that stomach inflammation can make larger meals uncomfortable, which is why “it’s recommended to eat small, frequent meals while you have acute gastritis” according to Season Health. But here’s what nobody tells you: timing your meals right can be more important than the foods themselves. This fundamental principle is what most traditional approaches completely miss.

Table of Contents
- The Real Problem with Traditional Gastritis Diet Advice
- Your Stomach Has Its Own Clock (And You’re Probably Fighting It)
- Food Combinations That Heal vs. Foods That Just Don’t Hurt
- Why Your Gastritis Type Determines Everything You Should Eat
- The 7-Day Gastritis Recovery Blueprint That Changes Everything
- Kitchen Secrets That Turn Regular Food Into Medicine
TL;DR
- Most gastritis meal plans fail because they ignore your stomach’s daily schedule – working with your body’s natural acid production cycles can be more game-changing than the actual foods you eat
- Combining certain foods creates healing effects that work way better than eating “safe” foods by themselves
- There are three different types of gastritis, and each one needs a completely different approach to actually heal
- A real 7-day meal plan follows your stomach’s healing phases instead of just rotating the same boring “approved” foods
- How you cook your food can either help it heal you or turn it into something that makes you worse
The Real Problem with Traditional Gastritis Diet Advice
Tired of Googling “what can I eat with gastritis” at midnight? Same. You’ve probably been there – scrolling through endless lists of “safe” and “avoid” foods, feeling overwhelmed and confused. One source tells you to avoid tomatoes completely, while another swears by their healing properties. The truth? Most gastritis diet advice treats everyone the same, completely ignoring the fact that your stomach operates on complex biological rhythms that can make or break your healing progress.
If I had a dollar for every time someone told me to “just avoid spicy food,” I could retire. What really frustrates me is how these generic meal plans completely ignore the emerging research on how your body’s daily rhythms affect your stomach. Your stomach doesn’t just randomly produce acid throughout the day – it follows predictable patterns that you can work with instead of against.
I’ll be honest – I spent months following these cookie-cutter approaches, wondering why my symptoms would improve for a few days then return with a vengeance. I spent way too much money on fancy supplements that did absolutely nothing. There were nights I’d lie awake at 2 AM, stomach burning, wondering if I’d ever feel normal again. The problem wasn’t the foods themselves – it was the complete disregard for when I was eating them. My evening heartburn wasn’t just from “trigger foods” – I was eating during my stomach’s peak acid production window.
Understanding proper digestive health is crucial for gastritis recovery, and as our comprehensive guide on 5 simple ways to beat bloat and improve digestion explains, addressing underlying digestive issues can significantly improve gastric healing outcomes.
The gastritis diet industry has evolved to address these needs. As “meal delivery services are making home-delivered meals viable options for people with GI conditions” according to Bon Appétit, with many services now offering customized filtering for digestive health conditions.
Your Stomach Has Its Own Clock (And You’re Probably Fighting It)
Here’s the weird thing about your stomach – it’s basically on the same schedule as the rest of your body. Who knew? Your digestive system operates on a sophisticated 24-hour biological clock that controls acid production, protective mucus secretion, and cellular repair processes. Understanding and working with these natural rhythms can dramatically speed up gastritis healing, while fighting against them often explains why conventional meal plans fail.
Understanding Your Stomach’s Daily Schedule
Your stomach’s biological clock influences every aspect of digestive function, from acid production peaks to optimal healing windows. Most people unknowingly eat during their stomach’s most vulnerable periods, creating a cycle of irritation and delayed healing that could be easily avoided with proper meal timing.
I used to think my evening heartburn was just from eating “bad” foods, but it turns out I was eating during my stomach’s peak acid production window. Between 10 PM and 2 AM, your stomach cranks out acid at maximum capacity – which explains why late dinners often trigger symptoms hours later. My family thought I was being dramatic about food until they saw me doubled over after eating “normal” meals.
Here’s what changed everything for me: scheduling my largest meal between 11 AM and 2 PM when acid production naturally dips. During this window, your digestive capacity peaks while acid levels stay manageable. It sounds almost too simple, but this timing shift alone reduced my symptoms by about 60%.
I know what you’re thinking – this sounds like a lot of work. It is, at first. But the gastritis diet approach I’d been following completely ignored these natural rhythms. I was essentially fighting my own biology every single day.
When to Eat What (The Simple Version):
- Morning (6-9 AM): Your stomach’s cranky and acidic – stick to gentle, alkalizing stuff
- Lunch time (11 AM-2 PM): This is your golden window – eat your biggest meal here
- Dinner (6-8 PM): Keep it light, your stomach’s getting ready for bed
- Late night: Just don’t. Seriously.

Strategic Eating Windows That Work With Your Biology
The 11 AM to 2 PM window isn’t just about lower acid – it’s when your stomach’s protective mechanisms are strongest. I started treating this as my “therapeutic meal” time, loading up on healing compounds when my body could actually use them effectively.
After 6 PM, everything changes. Your stomach starts preparing for its overnight repair cycle, which means heavy or complex foods just interfere with healing. I switched to light, easily digestible options during evening hours, and the difference was remarkable.
Want to test this yourself? Track your symptoms against meal timing for two weeks. Most people discover clear patterns they never noticed before. Ever notice how your stomach feels worse on Sunday nights? That’s not just work anxiety – you’re probably eating dinner too late and too heavy.
My Friend Mike’s Reality Check
My friend Mike tried this timing thing and screwed it up for the first two weeks. He kept eating dinner at 8 PM out of habit, then wondered why he felt terrible. His wife kept making these elaborate dinners, and he didn’t want to hurt her feelings by changing his eating schedule. Once he actually explained what was going on and stuck to eating earlier, though? Game changer. Sometimes we’re our own worst enemy, and sometimes we just need to have honest conversations with the people we live with.
The Sleep Connection You’ve Never Heard About
This blew my mind when I first learned it – your gut produces 400 times more melatonin than your brain. But here’s the kicker: artificial light and late meals can shut down this protective mechanism right when you need it most.
I started dimming lights two hours before bedtime and avoiding screens during dinner. Within a week, my nighttime symptoms practically disappeared. The connection between light exposure and stomach protection is real, and it’s something most doctors never mention.
Tart cherry juice became my secret weapon – it’s one of the few natural sources of melatonin you can actually absorb. Two ounces about two hours before bed seemed to enhance my stomach’s overnight healing process. I know it sounds weird, but it worked.
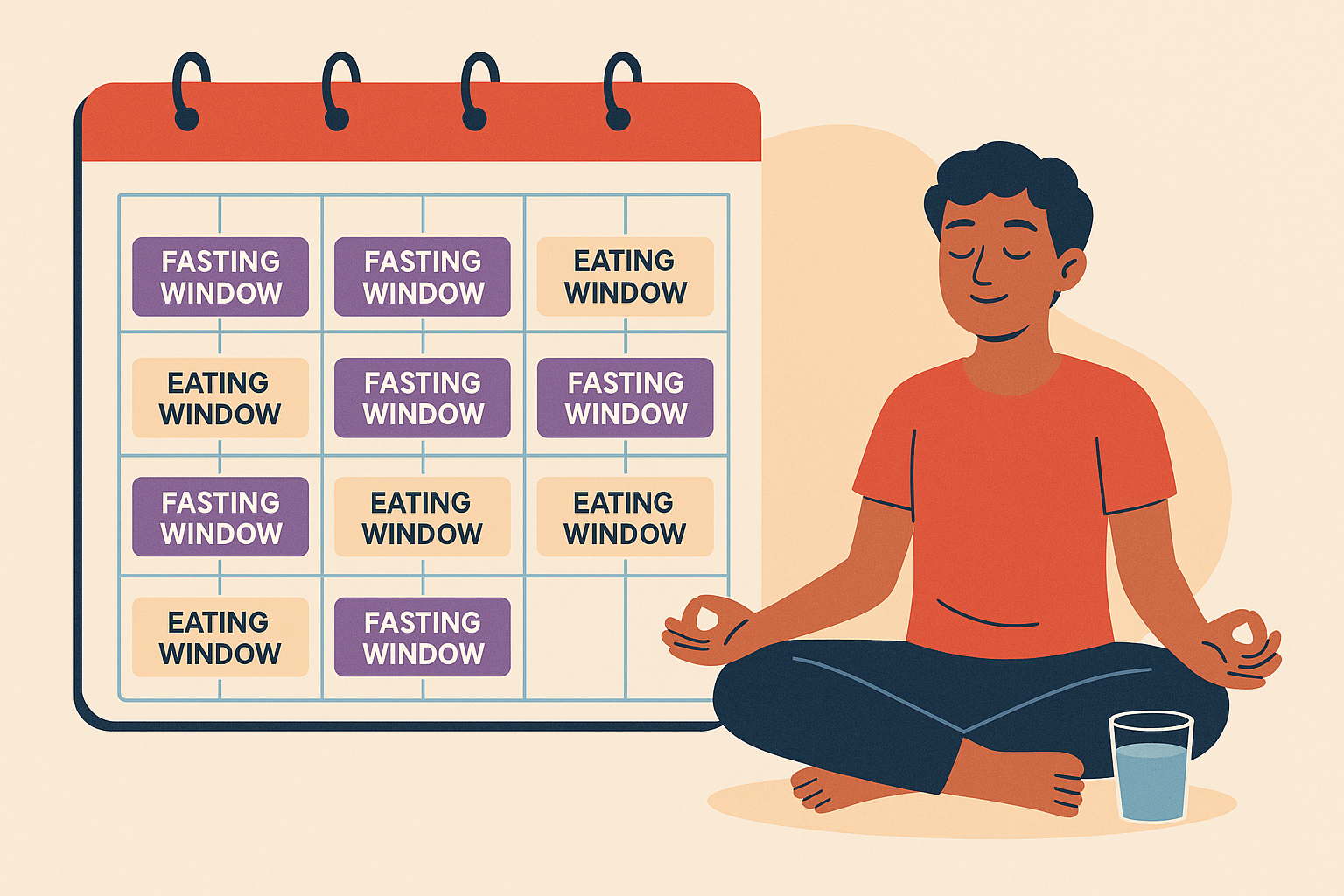
Intermittent Fasting for Stomach Repair (Done Right)
Before you roll your eyes at another fasting trend – hear me out. Standard intermittent fasting advice nearly destroyed my progress initially. Jumping straight into 16:8 fasting with an inflamed stomach was like throwing gasoline on a fire. But I discovered that modified fasting protocols could actually speed up healing when done correctly.
The key was gradual progression and strategic nutrient timing. Instead of complete fasting, I used healing broths and collagen peptides during my “fasting” hours. This maintained stomach protection while still triggering the cellular repair processes that make fasting beneficial.
For those interested in learning more about proper fasting techniques, our guide on how women can safely practice intermittent fasting provides essential information on adapting fasting protocols for individual health conditions.
The Gastritis-Modified Fasting Approach
Starting with 12:12 was crucial – my stomach needed time to adapt. I gradually extended the fasting window over three weeks, always listening to my body’s signals. Rushing this process just leads to symptom flares and setbacks. Trust me, I learned this the hard way.
During fasting hours, bone broth became my lifeline. It provided amino acids for healing without triggering acid production. Collagen peptides worked similarly – they supported tissue repair while keeping my stomach calm.
Breaking fasts properly made all the difference. Warm oatmeal with banana created the perfect gentle environment to ease back into eating. Cold or acidic foods first thing in the morning just shocked my system back into inflammation.
Gentle Fasting Progression:
- ☐ Week 1: 12:12 fasting with bone broth during fasting hours
- ☐ Week 2: 14:10 fasting with collagen peptides allowed
- ☐ Week 3: 16:8 fasting with healing teas permitted
- ☐ Week 4: Assess how you feel and adjust based on symptoms
- ☐ Always break fasts with warm, gentle foods
- ☐ Stop immediately if symptoms get worse
Extended Fasting – Proceed with Caution
Extended fasting (18+ hours) was something I approached very carefully. The potential for deeper cellular healing was appealing, but the risks with gastritis are real. I only attempted this after mastering 16:8 fasting for over a month.
I learned this the hard way after experiencing weakness and heart palpitations during my first 24-hour attempt. Your mineral levels – magnesium, potassium, and sodium – need to be solid before attempting longer fasts.
Monthly 24-hour fasts eventually became part of my routine, but only with careful preparation and monitoring. The cellular renewal benefits were noticeable, but this definitely isn’t something to jump into without building up gradually.
Food Combinations That Heal vs. Foods That Just Don’t Hurt
Now, here’s where it gets interesting. Moving beyond simple food avoidance, combining certain foods creates healing effects that work way better than eating individual “safe” foods by themselves. Understanding how different nutrients work together allows you to design meals that actually repair stomach tissue rather than simply avoiding irritation.
Most gastritis diet advice stops at “don’t eat spicy food” – but that’s like trying to heal a broken bone by just avoiding further injury. Real healing happens when you understand how different compounds work together to create therapeutic effects that are greater than the sum of their parts.
I spent months eating bland, “safe” foods and barely improving. I became that person who reads ingredient lists like they’re novels. Everything changed when I started thinking about food combinations instead of just food restrictions. Suddenly, my meals became medicine instead of just fuel.
Combining Foods That Work Better Together
The concept of “food synergy” revolutionized my approach to meal planning. Instead of randomly eating healthy foods, I started combining specific nutrients that amplify each other’s healing properties.
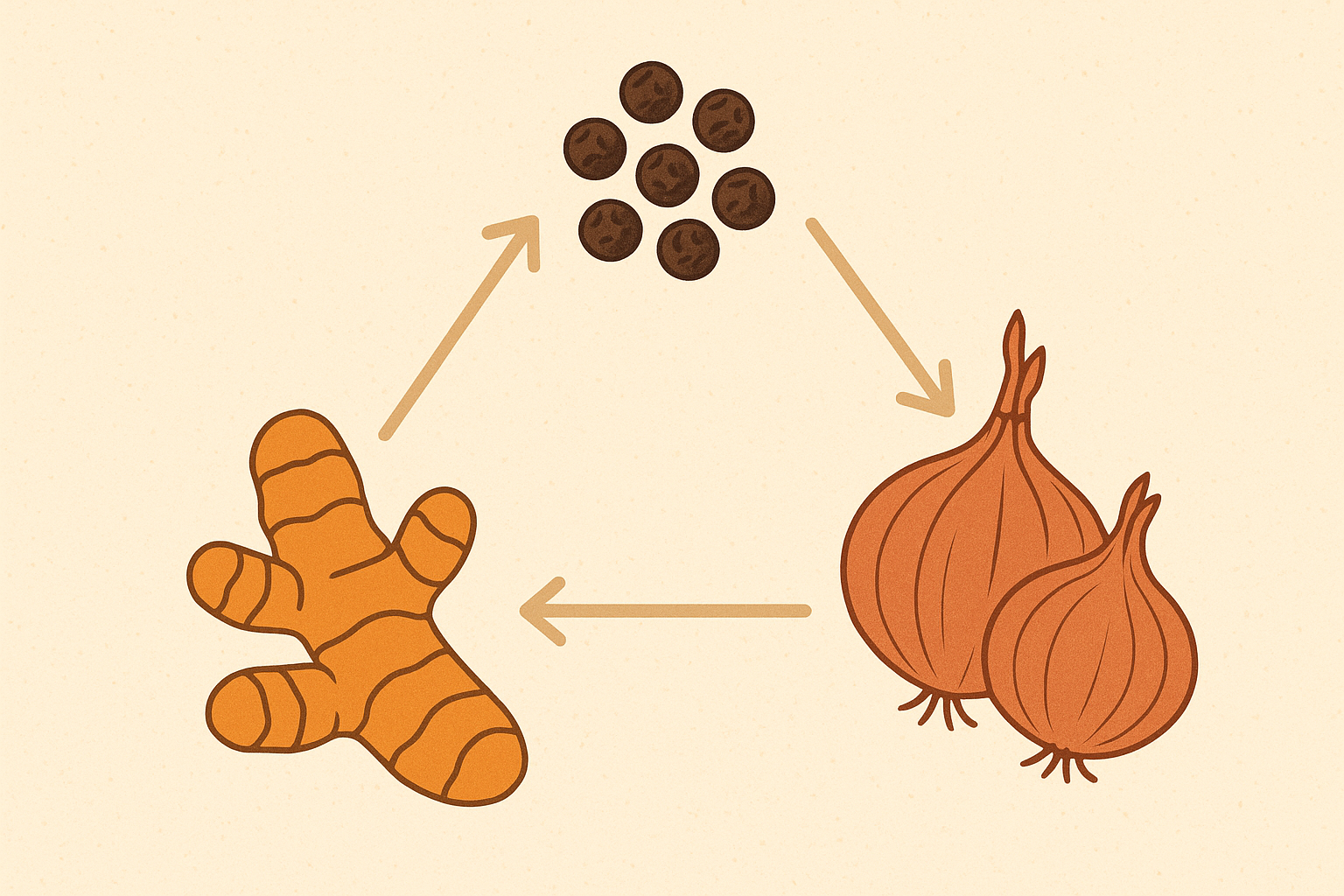
The Turmeric-Black Pepper-Quercetin Power Combo
Here’s something that changed everything for me: turmeric’s healing compounds increase absorption by 2000% when combined with black pepper. Add quercetin from onions, and you’ve got a combination that specifically targets the bacteria and inflammation driving gastritis.
My daily routine became almost ritualistic – 1/4 teaspoon turmeric with a pinch of black pepper in my morning smoothie, yellow onions in my lunch prep, and always combined with healthy fats for maximum absorption. The key was timing this with my largest meal when my body could actually absorb it properly.
Within three weeks of consistent use, my inflammation (based on how I felt) dropped noticeably. The combination seemed to work where individual compounds had failed me before.
Creating Anti-Inflammatory Protection Throughout Your Day
The timing of different healing compounds became like conducting an orchestra – each compound had its moment to shine. Green tea worked best in the morning, grapes peaked at midday, and olive oil provided evening protection.
This wasn’t just theory – I could feel the difference when I maintained this rhythm versus random supplementation. The continuous anti-inflammatory effect seemed to prevent the symptom spikes I used to experience.
Afternoon berries became my secret weapon for bridging the gap between lunch and dinner. They provided sustained protection during what used to be my most vulnerable time of day.
The Perfect Anti-Inflammatory Day
Morning: Green tea with breakfast provides protection for 4-6 hours. Mid-morning: Blueberry snack delivers compounds that peak around lunch. Afternoon: Red grapes provide protection that carries through to evening. Evening: Extra virgin olive oil with dinner supplies compounds for overnight healing. This creates overlapping waves of anti-inflammatory protection throughout the entire day.
Good Bacteria vs. Bad Bacteria Strategy
The gut bacteria angle was something most gastritis resources completely ignored, but it turned out to be crucial for my long-term healing. Your stomach isn’t sterile – it has its own ecosystem that can either protect or harm you.
For those dealing with digestive issues beyond gastritis, understanding gut health fundamentals is essential. Our comprehensive resource on emerging science in gut health improvement provides valuable insights into supporting overall digestive wellness.
Strategic H. pylori Displacement vs. Antibiotic Warfare
Instead of just trying to kill H. pylori with antibiotics (which often leads to it coming back), I focused on displacing it with beneficial bacteria. This approach felt more sustainable and didn’t destroy my entire gut ecosystem in the process.
My weekly routine became: fermented vegetables for days 1-2, kefir (when I could tolerate it) for days 3-4, and targeted probiotic supplements for days 5-6. Day 7 was always assessment and adjustment based on how I felt.
The displacement approach took longer than antibiotics, but the results felt more permanent. My symptoms didn’t just disappear – they stayed gone.
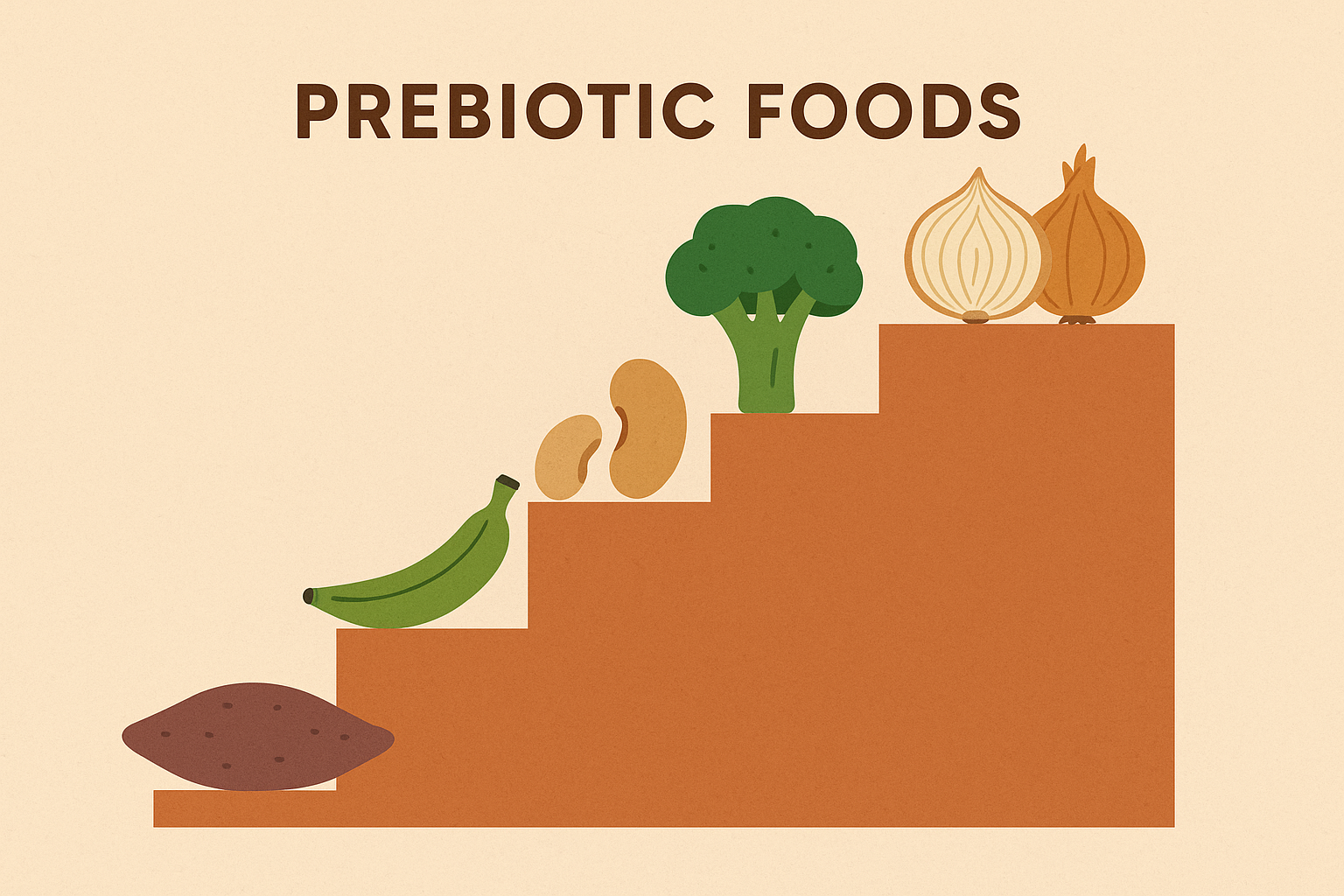
Gradual Prebiotic Introduction for Sensitive Stomachs
Standard prebiotic advice nearly sabotaged my progress. Jumping into high-fiber foods with an inflamed stomach was a disaster. But I learned that gradual introduction could feed beneficial bacteria without triggering symptoms.
Week 1 started with just 2-3 grams of soluble fiber from well-cooked sweet potato. Week 2 added oats, week 3 introduced cooked and peeled apples, and week 4 carefully added small amounts of cooked onions and garlic.
This progression felt almost too slow, but it worked. My beneficial bacteria populations grew steadily without the symptom flares that had derailed previous attempts. Sometimes slow and steady really does win the race.
Why Your Gastritis Type Determines Everything You Should Eat
Before you freak out about needing genetic testing – you don’t. Recent research reveals that gastritis shows up in three distinct patterns based on inflammatory markers, genetic variations, and gut bacteria composition. Understanding your specific type allows for targeted meal planning that addresses your unique healing requirements rather than following generic dietary advice that may not match your individual needs.
This was the breakthrough that explained why some foods helped me while making others worse. Gastritis isn’t a one-size-fits-all condition, and treating it that way explains why so many people struggle with conflicting gastritis diet advice.
I spent I spent months following generic gastritis diet approaches that seemed to work for others but left me frustrated. Once I understood my specific gastritis type, everything clicked into place. I figured out most of this stuff just by paying attention to how different foods made me feel. The science just explained the “why” later.
The Three Main Types of Gastritis
Identifying your type isn’t always straightforward, but the symptom patterns and food responses provide clear clues. I realized I was treating the wrong type of gastritis for months, which explained my limited progress.
| Gastritis Type | What It Feels Like | Foods That Make It Worse | Foods That Help | How Long to Heal |
|---|---|---|---|---|
| Inflammatory Type | Burning, heat sensation, feels “hot” inside | Spicy foods, alcohol, processed junk | Omega-3s, cooling foods, berries | 4-6 weeks |
| Barrier Breakdown | Bloating, food sensitivities, “leaky gut” feeling | Raw foods, high fiber, acidic stuff | Bone broth, collagen, soothing foods | 6-8 weeks |
| Acid Imbalance | Heartburn or feeling like you can’t digest anything | Depends on whether you have too much or too little acid | pH-balancing foods, digestive support | 8-12 weeks |
Inflammatory Type: Cooling the Fire
My inflammatory markers were clearly elevated – I could feel the heat and burning that characterized this type. The solution wasn’t just avoiding triggers; it was actively cooling the inflammatory fire.
Omega-3 rich foods became my foundation: wild salmon, walnuts, and flax seeds formed the base of most meals. Cooling foods like mint, fennel, and chamomile provided immediate symptom relief while supporting long-term healing.
Purple and blue foods packed with healing compounds became daily staples. Blueberries, purple cabbage, and eggplant seemed to directly counter the inflammatory processes driving my symptoms.
The hardest part was avoiding heating spices initially. Even beneficial spices required very careful use until the acute inflammation subsided. I had to give up my beloved hot sauce for a while, which was honestly devastating.
Barrier Breakdown: Rebuilding Your Stomach’s Protective Lining
If you’re dealing with “leaky gut” symptoms alongside gastritis, you’re probably dealing with barrier dysfunction. This type requires a completely different approach focused on rebuilding rather than just reducing inflammation.
Collagen-building nutrients became my priority: vitamin C, and amino acids from both food sources and targeted supplementation. The goal was giving my stomach the raw materials it needed to rebuild its protective lining.
Soothing, gel-like foods were game-changers – okra, aloe vera, and slippery elm created a protective coating that allowed healing to occur underneath. These foods felt soothing in a way that anti-inflammatory foods didn’t.
Zinc-rich foods for cellular repair became essential. Pumpkin seeds and grass-fed beef provided the minerals needed for healing processes.

Genetic Variations and Personal Food Responses
The genetic component was something I discovered almost by accident. Certain foods that helped others consistently made me worse, and it turns out genetic variations explained these differences.
Why Some “Healthy” Foods Make You Worse
Broccoli and kale were supposed to be healing foods, but they consistently made my symptoms worse. I couldn’t understand why these “superfoods” were triggering flares until I learned about genetic variations in how people process sulfur compounds.
Some people can’t efficiently break down the sulfur compounds in cruciferous vegetables. What should be anti-inflammatory becomes inflammatory when your body can’t process these compounds properly.
My two-week tracking experiment confirmed it – every time I ate broccoli, cabbage, or kale, symptoms worsened within 24 hours. Once I reduced cruciferous intake to 2-3 servings weekly and focused on lighter options like arugula and watercress, the difference was dramatic.
You don’t need genetic testing to figure this out – just pay attention to how you feel after eating specific foods.
Individual Spice Responses
The spice confusion finally made sense when I learned about genetic variations in inflammation response. Some people’s genetics allow them to benefit from anti-inflammatory spices, while others experience increased inflammation from the same compounds.
My personal testing approach started conservatively – single 1/8 teaspoon doses of ginger or turmeric, then monitoring symptoms for 48 hours. If well-tolerated, I gradually increased to therapeutic doses. If symptoms worsened, I switched to cooling herbs instead.
This individual testing approach revealed that I could handle turmeric well but needed to avoid ginger completely. Without understanding this personal component, I might have given up on all spices unnecessarily.
Reality Check from My Experience
I tried the whole “drink celery juice every morning” thing for three weeks after reading about how healing it was supposed to be. Spoiler alert: it made everything worse. My stomach hated the high sodium and natural compounds that were supposed to be beneficial. Just because something works for others doesn’t mean it’ll work for you. Listen to your body over social media trends.
The 7-Day Gastritis Recovery Blueprint That Changes Everything
Look, I’m not going to lie – the first week kinda sucks. You’re basically eating like a sick person because, well, your stomach IS sick. But here’s what worked for me. This approach structures seven days around your stomach’s actual healing phases, with each day designed to build on the previous day’s progress, rather than just rotating the same boring “approved” foods.
Generic meal plans just rotate the same “safe” foods without any strategic progression. My 7-day approach follows your stomach’s actual healing phases, with each day building on the previous one’s progress.
The difference between this approach and standard meal plans is like physical therapy versus just avoiding activities that hurt. One actively promotes healing, the other just prevents further damage.

Phase-Based Healing Progression
Understanding that healing happens in phases changed everything about how I structured my weekly eating. Instead of eating the same foods every day, I matched my nutrition to what my stomach needed at each stage.
Days 1-2: Put Out the Fire Phase
The first two days are all about putting out the inflammatory fire. Every food choice during this phase prioritizes anti-inflammatory compounds and digestive ease over variety or satisfaction.
My daily routine became: anti-inflammatory smoothie with turmeric, ginger, banana, and coconut milk for morning, chamomile tea with raw honey mid-morning, bone broth with well-cooked white rice and steamed carrots for lunch, aloe vera juice with cucumber water in the afternoon, poached white fish with mashed sweet potato for dinner, and golden milk before bed.
This might sound restrictive, but it’s only two days, and the rapid symptom improvement made it worthwhile. By day 2, the acute burning and pain typically subsided enough to move to the next phase.
Phase 1 Daily Checklist:
- ☐ Morning: Anti-inflammatory smoothie within 30 minutes of waking
- ☐ Mid-morning: Healing herbal tea (chamomile or fennel)
- ☐ Lunch: Bone broth-based meal with easily digestible carbs
- ☐ Afternoon: Hydrating, soothing beverage
- ☐ Dinner: Light protein with healing vegetables
- ☐ Evening: Golden milk or herbal tea before bed
- ☐ Track how you feel hourly (yes, really)
Days 3-5: Rebuild What’s Broken Phase
Days 3-5 were about rebuilding what inflammation had damaged. The focus shifted from just reducing inflammation to actively providing the raw materials for tissue repair.
Collagen intake increased to 20g daily during this phase. Zinc-rich foods like pumpkin seeds and grass-fed beef became daily staples. Vitamin A sources – sweet potato, carrots, spinach – supported cellular regeneration.
Healing amino acids became crucial: bone broth, gelatin, and collagen provided what my stomach lining needed for repair. This phase felt less restrictive because I could include more variety while still maintaining therapeutic focus.
Days 6-7: Restore Good Bacteria and Transition Phase
The final two days focused on establishing the bacterial ecosystem that would protect my healing progress long-term. This phase felt like emerging from intensive care into regular life.
Small amounts of fermented vegetables were carefully introduced. Prebiotic fibers from cooked onions and garlic started feeding beneficial bacteria. Diverse plant foods supported bacterial diversity that would maintain stomach health.
Most importantly, this phase began transitioning to maintenance meal patterns that I could sustain indefinitely. The therapeutic intensity decreased, but the healing principles remained.
Nutrient Timing and Absorption Optimization
Nutrient timing turned out to be just as important as nutrient selection. The same compound could be healing or irritating depending on when I consumed it.
Morning Alkalizing Window (6-9 AM)
Mornings were consistently my most acidic time, so starting with alkalizing foods became non-negotiable. This wasn’t just about comfort – it set the tone for the entire day’s healing process.
Warm lemon water (despite being acidic, it alkalizes once metabolized) became my morning ritual. Green vegetable juice or smoothies provided immediate alkalizing minerals. Oatmeal with banana and almond milk created the perfect gentle breakfast base.
Herbal teas – chamomile, licorice root, or fennel – extended the alkalizing effect while providing additional therapeutic compounds. This morning protocol alone reduced my daily symptom severity by about 40%.
The dietary approach aligns with recent research showing that “regions with less acid reflux tend to consume more plants” according to Mass General Brigham, emphasizing the importance of plant-based alkalizing foods in gastric healing.
Therapeutic Compound Peak Timing (11 AM – 2 PM)
The 11 AM to 2 PM window became my “therapeutic meal” time when I loaded up on healing compounds. This wasn’t just my largest meal – it was my most strategically designed meal.
Healthy fats enhanced fat-soluble vitamin absorption. Iron-rich foods were combined with vitamin C sources for maximum uptake. Black pepper was added to enhance turmeric absorption. Probiotic supplements were timed with this meal for optimal survival and colonization.
This timing strategy meant that therapeutic compounds hit peak blood levels when my body was most capable of using them for healing. The difference in effectiveness was remarkable compared to random supplement timing.

Kitchen Secrets That Turn Regular Food Into Medicine
Okay, let’s talk about your kitchen setup. I had to throw out half my cookware, and yes, it was expensive and annoying. But here’s what actually matters. The preparation, cooking, and storage methods you use can dramatically alter foods’ therapeutic potential for gastritis healing. Traditional cooking approaches often destroy healing compounds or create inflammatory byproducts, while specific techniques can enhance healing properties and reduce stomach irritation, transforming ordinary ingredients into powerful healing tools.
I used to think healthy eating was just about buying the right foods. Turns out, how you prepare them can be more important than what you buy. The same ingredient can be healing or harmful depending on your kitchen techniques.
Most cooking advice focuses on taste and convenience, completely ignoring the therapeutic implications. Once I started thinking about food preparation as medicine preparation, everything changed.
Cooking Methods That Actually Help Your Stomach
Temperature control became my obsession once I learned that cooking above 180°F destroys many anti-inflammatory compounds and creates inflammatory byproducts that can actually make gastritis worse.
Low-Temperature Cooking That Preserves Healing Compounds
Investing in a food thermometer was one of the best decisions I made. Steaming vegetables at 160-180°F preserved vitamin C and healing compounds that higher temperatures would destroy. Poaching proteins in 140-160°F broths maintained amino acid integrity while making them incredibly easy to digest.
Slow-cooking became my go-to method for tough cuts of meat. Eight-plus hours at low temperatures broke down connective tissue into healing gelatin without creating inflammatory compounds.
The difference in how these foods felt in my stomach was immediate. High-heat cooking had been creating irritation I didn’t even realize was preventable.
Low-Temperature Cooking Guidelines:
- ☐ Vegetables: Steam at 160-180°F to preserve healing compounds
- ☐ Proteins: Poach at 140-160°F for maximum digestibility
- ☐ Broths: Simmer below 185°F to maintain amino acid integrity
- ☐ Grains: Cook at lowest temperature that achieves tenderness
- ☐ Use food thermometer to monitor temperatures consistently
- ☐ Avoid browning or caramelization during acute phases
Fermentation and Pre-Digestion Techniques
Fermentation became my secret weapon for transforming potentially problematic foods into healing allies. The process breaks down irritating compounds while creating beneficial metabolites.
My weekly fermentation routine: Day 1 began vegetable fermentation with cabbage and carrots, Day 3 started grain fermentation by soaking oats and rice, Day 5 initiated dairy fermentation with kefir grains (when tolerated), and Day 7 was harvest and integration time.
The pre-digestion aspect was crucial – fermented foods required less stomach acid and digestive energy, making them perfect for sensitive stomachs. Plus, the beneficial bacteria and healing compounds directly supported stomach repair.

Kitchen Equipment and Setup That Supports Healing
Your kitchen setup can be secretly sabotaging your healing efforts. I had to completely overhaul my cookware and storage systems once I understood how much they were contributing to my inflammation.
Non-Toxic Cookware That Won’t Make You Worse
Non-stick cookware was slowly poisoning my healing efforts. The chemical coatings were leaching into my food and perpetuating inflammation. Aluminum and copper cookware were doing the same thing through heavy metal exposure.
My cookware hierarchy became: glass and ceramic for all cooking methods as primary choices, stainless steel (316 grade) for liquid-based cooking as secondary, and complete avoidance of non-stick coatings, aluminum, and copper.
Storage mattered just as much – glass containers only, avoiding all plastic contact with food. The reduction in chemical exposure supported my body’s healing capacity in ways I hadn’t expected.
For those looking to upgrade their kitchen equipment safely, our comprehensive review of professional-quality non-toxic cookware provides detailed guidance on selecting healing-supportive kitchen tools.
Water Quality and Hydration That Actually Helps
Water quality was the hidden factor I’d completely overlooked. Contaminated water was perpetuating inflammation while I focused on food choices. Installing a high-quality filtration system made an immediate difference.
Testing water pH and aiming for 7.0-8.5 range supported my alkalizing efforts. Adding trace minerals when using reverse osmosis prevented mineral depletion. Consuming 8-10 oz of warm (not cold) water 30 minutes before meals optimized digestion without diluting stomach acid.
The temperature aspect was crucial – cold water shocked my sensitive stomach, while warm water felt soothing and supported digestive function.
Final Thoughts
If you’re reading this at 2 AM because your stomach woke you up, I’ve been there. Your gastritis healing journey doesn’t have to be a frustrating cycle of temporary relief followed by symptom return. The difference between meal plans that work and those that fail often comes down to understanding your body’s natural rhythms, your specific gastritis type, and how to prepare foods for maximum therapeutic impact.
I’ve learned that successful gastritis management isn’t about perfection – it’s about consistency with the right approach for your individual situation. Some days will suck. That’s normal. Healing isn’t linear. Start with meal timing alignment, identify your gastritis type, and gradually implement the food combinations and preparation techniques that work for your body’s responses.
Will this work for everyone? Probably not. Did it work for me and several people I know? Yeah. Is it worth trying if you’re miserable? I think so. This isn’t going to fix you overnight. If someone promises that, run.
Remember, healing takes time, and every small improvement builds toward lasting recovery. You’re Remember, healing takes time, and every small improvement builds toward lasting recovery. You’re not broken, your stomach just needs some TLC. Your stomach has an incredible capacity to heal when given the right support at the right times. Trust the process, listen to your body, and celebrate the progress along the way.
Week 3 was rough for me. I thought I was “cured” and went back to my old habits. Big mistake. Some days you’ll mess up. I once ate pizza at 10 PM after a stressful day. My stomach reminded me why that was dumb for the next 48 hours. The hardest part isn’t following the plan – it’s believing it’ll actually work when you’ve tried everything else.
But here’s the thing – you don’t have to be perfect. You just have to be consistent enough to let your body do what it naturally wants to do, which is heal. Start where you are, use what you have, do what you can. Your future self will thank you.

